Awake, Yet Asleep

The clinking of medical tools slowly fades out as the patient lies on the operating table, impatiently waiting for the process to conclude. The anesthesiologist receives thee cue, and then the patient slowly drifts into a peaceful dream state. “Count down backwards for me, 10…9…8…7…6…5…4…3…2…1.”
Only minutes before, the patient was completely aware of his or her surroundings and braced oneself for the next step in which one was promised – that he or she wouldn’t remember.
Laying unconscious on a cold steel table, waiting for surgeons to carve into the skin, one suddenly starts to hear movement. The shuffling voices of doctors discussing their first move sounds strangely louder than before.
The patient start to panic. “Wait, am I supposed to be hearing this right now?”
As the doctor inches closer and closer with scalpel in hand, the patient’s nerves react faster than ever before and they feel every concentrated cut and pull.

As loud as one tries to shriek for help, the only person in the room that can hear it, is you. All your yelling and protests are contained within your own brain. You lie paralyzed on the operating table, unable to grab the doctor and let them know you are still awake and can feel everything. This could last for hours.
Afterwards, you may have the courage to notify the hospital that they were mentally awake throughout the entire procedure, but in many situations, hospital staff simply don’t believe the victim.
This temporary condition, referred to as anesthesia awareness, is difficult to prove but has a permanent, traumatic effect on its victims.
Anesthesia awareness affects less than 1 percent of U.S patients given general anesthesia. Whether it is dental surgery or organ transplantation, a form of anesthesia is always present in the operating room. General anesthesia and local anesthesia are the two types of anesthesia used when undergoing certain medical procedures. Victims who experience anesthesia awareness are normally under general anesthesia. General anesthesia is most commonly a combination of intravenous drugs and inhaled gasses. General anesthetics are known to alter the Central Nervous System and leave patients in an induced coma state.
According to Medical News Today the specific areas of the (CNS) that are affected are:
- Cerebral cortex: the brain’s outer layer involved in tasks relating to memory, attention, perception among other functions
- Thalamus: roles include relaying information from the senses to the cerebral cortex and regulating sleep, wakefulness and consciousness
- Reticular activating system: important in regulating sleep-wake cycles
- Spinal cord: passes information from the brain to the body and vice versa. It also houses circuitry that controls reflexes and other motor patterns.
Some surgeries that require general anesthesia include organ transfers, colonoscopies, bone fracture repairs, breast augmentation, buttock implants and rhinoplasty.
Local anesthesia is different from general anesthesia, as the patient being injected with the local anesthetics is fully awake, and is only numb in a specific area. Some procedures done with local anesthetics include Botox injections and certain dental extractions.
An experience that is commonly confused with anesthesia awareness is simply waking up during surgery. When a patient awakens during surgery, their mobile abilities are fully operative, and they are able to speak.
These individuals simply were not administered the correct amount of anesthesia and their brain allowed the patient to be released from the trance-like state. This can be easily resolved with an increased, but safe amount of anesthesia.
The victims that experience anesthesia awareness commonly “go under” because many medical professionals believe that the individuals are confusing their experience with simply waking up, or just having a dream.
During many surgeries that require general anesthesia, a breathing tube is inserted through the individuals mouth, down their throat. This step is a necessity during surgery to accurately monitor the patient’s breathing, as it can be difficult or impossible for patients to force themselves to speak, and vomiting under general anesthesia can lead to death.
Although many victims of anesthesia awareness tend to stray from talking about their traumatic experience, some people have found a community on YouTube where they have been more open.
Youtuber Katrina Sherwood, also known as Katrinaosity, uploaded a video earlier this year to talk about her personal experience with anesthesia awareness.

Sherwood explains in the video that she underwent an adrenalectomy for a Pheochromocytoma. In layman’s terms, this operation is an organ removal surgery that removes one or more of the adrenal glands. The adrenal glands are two small organs located above each kidney. Sherwood had to get a tumor removed from the one affixed above her right kidney.
The 26-minute-long video shows Sherwood’s vulnerability when recalling the event of horror.
“It felt like someone was taking a PVC pipe and shoving it into my arm. In reality, the cannula was pretty small,” Sherwood states.
Sherwood goes on to mention when the catheter went down her neck arteries into her heart. “The sensation is what I imagine it would be like to be injected with poison,” Sherwood states. “As it entered my heart, while it was moving in there, the heart really doesn’t quite beat, I just felt vibration.”
Sherwood also goes on to explain the most painful aspect of the surgery, when the doctors made “small” incisions on her abdomen. “I started to feel burning, and then I started to smell burning, and it was my flesh,” Sherwood recalls. “When I started smelling it, a couple seconds later I started tasting it.”
Sherwood continues on to vividly describe the potent smell of her burning flesh as a mixture between burning hair and barbeque without the sauce. Sherwood concludes the video by mentioning the most important conscious decision she has made. She talks about the two options she had in the moment which was to leave her body peacefully or simply “ride it out.”
Sherwood’s comments shed some light on the extent that one’s mind can reach in that type of scenario. She wanted to leave her body because it seemed like the easier way out, but believes God led her to her decision. “I guess I was talking to God and he told me, either way is okay.”
Following this YouTuber’s display of vulnerability, another victim, Blaize Morgan also known as It’s Blaize, also shared her experience with anesthesia awareness.
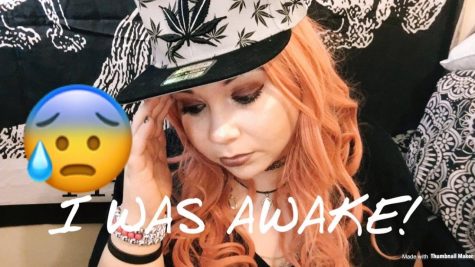
Morgan experienced awareness when undergoing an oral surgery. In the video, she also mentions how she has a massive phobia of the dentist and is highly prone to anxiety attacks, panic attacks and sleep paralysis.
Morgan goes on to say how resistant she is to medication due to her experience with previous surgeries and the doctors’ difficulties putting Morgan into a complete unconscious state.
“I was ‘under’ for two and a half hours…it felt like two and a half days.” Morgan continues to reignite the image in her mind. “I was looking up at the ceiling trying to count how many tiles there were.”
Morgan then mentions how after the surgery concluded and she was “awakened,” that none of the medical professionals believed she was telling the truth, and avoided admitting to their wrongs.
“How do I know you were saying this to your receptionist, you were saying this to your nurse, you were saying this to the anesthesiologist? How do I know what this smelled like, tasted like, how do you explain that I know everything that was going on but I was… asleep?”
Morgan refuses to undergo any type of surgery that requires general anesthesia after her experience.
Despite the fact that Morgan and her family paid an extra $2000 for the anesthesiologist, since the dental office didn’t provide one, Morgan’s comments on her common experience with sleep paralysis is a topic that would traumatize any viewer.
Sleep paralysis is one of the hidden, pre-existing conditions that should always be taken into consideration by any doctor or certified anesthesiologist before surgery. It is a necessity for the medical team to identify whether the candidate has any pre-existing conditions that will alter the effect of anesthesia on their body to avoid an anesthesia awareness.
Mercy College’s Program Director for the Undergraduate Nursing Program, Patricia Sutton, believes victims that suffer from sleep paralysis, anxiety disorder or depression should also be highly evaluated before surgery, just as patients with pre-existing conditions such as asthma, cancer, or previous drug use/addiction would be evaluated.
Sutton has years of experience in the Post Anesthesia Care Unit, and feels that medical professionals should take this possible patient experience more seriously. Sutton prepares her undergraduate nursing students with specific guidelines they can abide by to assist medical professionals while working closely with anesthesia, and she believes that brain monitors are most helpful in identifying if a patient is mentally conscious.
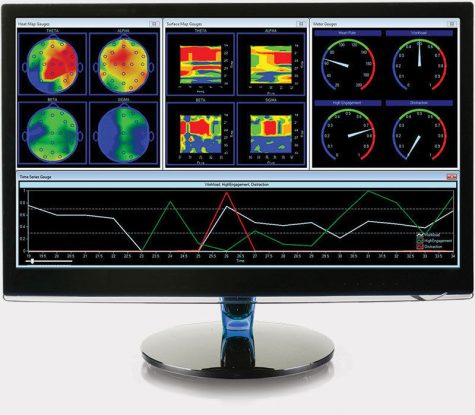
In all operating rooms, a person’s vital signs should be strictly monitored. Those vital signs being: body temperature, blood pressure, pulse (heart rate), and breathing rate (respiratory rate).
Unfortunately, brain monitors are not available in every hospital due to their high price tag (up to $3,000 if one’s medical insurance doesn’t cover it.) If every hospital had the funding and ability to engage in ongoing EEG tests on an individual under general anesthesia, this intraoperative awareness can be better avoided.
According to Kids Health Organization the electroencephalogram (EEG) tracks and records brain wave patterns. Small metal discs with thin wires (electrodes) are placed on the scalp, and then send signals to a computer to record the results. Through this machine, doctor’s can recognize any alteration in brain activity that disrupts the normal pattern.
Although brain monitors would be a tremendous asset to the operating room, there are occasions where the use of faulty medical tools can attribute to anesthesia awareness in a patient.
It is imperative to resupply the operating room with tools that are not expired, or have been tested for accuracy before each time it is going to be used on a patient.
Only about 10 years ago has the topic of anesthesia awareness prominently surfaced media attention.
The 2007 film Awake is the first time that intraoperative awareness is depicted to the public eye as a real experience that many individuals endure.
The film, which stars Hayden Christensen as the victim undergoing anesthesia awareness during heart surgery, Jessica Alba as his spouse, and Terrence Howard as the certified surgeon.
Some reviews say the film focused more on the steamy, backstabbing plot within characters instead of the full experience of anesthesia awareness. Despite the opinionated comments, it was the first film to explore some aspect of the horrifying medical truth.
According to the Mayo Clinic organization, 1 or 2 people in every 10,000 under general anesthesia, experience the traumatic horror of unintended intraoperative awareness.
Although there are many steps that medical professionals can abide by before surgery, there is never an 100 percent guarantee this won’t happen to even the most monitored patient.

Nicole is from The Bronx and is a journalism major at Mercy College. Her hobbies include discovering new places to eat on a budget, photography, listening...




